SDG 3: Good Health and Wellbeing

Health does not mean the absence of disease or infirmity, but is a state of complete physical, mental, and social well‑being (World Health Organization/WHO). It encompasses both well‑being and the overall living conditions of people. Health status, quality of life, and life expectancy are influenced not only by medical care but above all by economic factors and social living conditions.
Health Inequality
Studies show that health inequality has remained largely stable over the past 20 years and has even increased in some areas. People living in poverty or on the run often lack adequate medical care. Individuals suffering from malnutrition, severe physical strain, or psychological stress (e.g., due to harmful working or environmental conditions) become ill more quickly. Those who cannot read or understand medication leaflets, instructions, or information about health care and preventive services cannot adequately make use of them. Thousands of newborns, young children, and adults fall ill and die daily from preventable and treatable diseases. According to current projections, one‑third of the world’s population will have no access to essential health care by 2030.
Research also shows that in Germany, people from higher socio‑economic groups are healthier and have a longer life expectancy than those with lower education, income, and occupational status. There are also class-specific differences in health and disease-related behaviors, e.g., in diet, physical activity, or the use of preventive and care services, which contribute to health inequality and differences in mortality.

Globalization of Health Risks
The coronavirus pandemic acted like a magnifying glass for inequalities in health care worldwide. This was evident, for example, in the unequal distribution of and access to vaccines, in the differing courses of the COVID-19 pandemic in richer and poorer countries, and in the disparities between wealthier and poorer regions within individual countries. Lockdowns, supply chain bottlenecks, and overburdened health systems exacerbated existing problems and wiped out previously achieved development progress: from interruptions in vaccination campaigns and the supply of essential medicines to the absence of medical personnel and inadequate health care for newborns, pregnant women, and mothers. Due to the COVID-19 crisis, essential medicines for AIDS, malaria, and tuberculosis are also lacking.
But it is not only global pandemics—also increasingly apparent are the health consequences of global warming, the threat to food security for large parts of the world population due to climate change, the marketing and profit interests of international agribusiness corporations and food speculation, the loss of the biological (genetic) diversity necessary for all of our survival, and the global system of patent rights on medicines, as well as our collective dependence on international drug production. All of this clearly shows that, and to what extent, health depends on social inequality, power asymmetries, resource distribution, and governance structures.
To this day, global health policy reflects historically rooted inequalities and is largely shaped by the hegemonial interests of Western European and North American institutions and governments. In this context, some speak of a “medical neo-colonialism” (Holst 2019).

Poverty-Related Disease
Almost half of the world’s population lacks access to health care due to insufficient financial resources; in rural areas, the proportion is even higher. In many countries, patients must pay for medical treatment and medications out of pocket, without reimbursement from health insurance. The result is so-called poverty-associated diseases: people become ill or die because they cannot afford the necessary medications.
The situation is further exacerbated by the strict policies and so-called structural adjustment reforms of the International Monetary Fund (IMF). Debt burdens and severe austerity measures to reduce budget deficits have led in many countries (e.g., Chad, Cameroon, Sri Lanka, but also Greece) to major cuts in public health spending, resulting in a noticeable deterioration of health care for the population and a proven increase in child mortality.
The UN Sustainable Development Goal 3
SDG 3 aims to ensure healthy lives and promote well-being for all people of all ages, everywhere in the world.
The targets under SDG 3 are ambitious: for example, preventable deaths of newborns and children under five should be reduced to zero by 2030, global maternal mortality reduced, universal access to sexual and reproductive health services—including family planning, information, and education—guaranteed, the epidemics of AIDS, tuberculosis, and malaria fully overcome, and access to quality essential health services as well as safe, effective, quality, and affordable essential medicines and vaccines for all ensured.
To strengthen public health systems and improve international cooperation in the health sector, a specific target (SDG 3.8) was established to build or reinforce public health systems and ensure universal health coverage for all.
The greatest challenges to achieving these goals include the COVID-19 pandemic and global warming.
The content of SDG 3 provides—especially from a medical perspective—a comprehensive yet still limited view of health and well-being. Aspects such as the promotion of social justice and democratic participation or the elimination of poverty as a structural condition for disease are not explicitly formulated as goals. Already in 1978, the WHO developed a much broader concept of primary health care (Alma-Ata Declaration, 1978), which, however, over the following decades, was reduced by influential global health actors to economic interests, marketability, and profitable medical interventions.
Global Health, One Health, Planetary Health
Over the past two decades, global health policy has become one of the most important areas of foreign and security policy. It encompasses not only individual clinical care and prevention for populations but also engagement with transnational issues. Political concepts of global health are not limited to cross-border health problems in the narrow sense but include factors such as food security, migration, urbanization, climate change, inequality, and power structures. It is a holistic, transdisciplinary, and human-rights-based approach aiming for “health for all.”
The One Health approach is based on the understanding that human, animal, and environmental health are closely interconnected. It describes a collaborative and transdisciplinary approach in which many sectors and actors work together at local, regional, national, and global levels. It particularly considers the interconnections between humans, animals, plants, and their shared environment to better understand and appropriately address the emergence of global health risks (for example, zoonoses).
The broader concept of Planetary Health explicitly incorporates the health impacts of human activity on life in the biosphere. Planetary Health places humans—not just their health—at the center and addresses the reduction of health inequalities caused by income, education, gender, and living environment.
A similar argument is made by proponents of the Health for Future movement, which follows the motto: Health requires climate protection!

Whichever of these concepts guides political action, one thing becomes clear: health must be understood in a comprehensive sense as a rights-based, universal good.
Health is a human right!
Core Goal of Global Health Policy: Overcoming existing global inequalities
Strategies to fight poverty and reduce socio-economic inequality are central to enforcing the right to health.
“As important as good medical care is, it has less influence on people’s health than their living conditions. Without proper consideration of the social determinants of health—the distribution of income, living and working conditions, education, environment, and other societal factors—it is not possible to sustainably improve the health of the world’s population” (Holst 2019).
Global health therefore requires:
- More health promotion rather than a disease-driven system
- Good working and income conditions
- Equal opportunities
- Reduction of socio-economic inequality
- Food sovereignty
- Responsible environmental policies
- Social security, peace, democracy, and participation
In September 2019, a so-called Global Action Plan (GAP) for healthy lives and well-being for all was presented on the sidelines of the 74th UN General Assembly in New York. The goal of the GAP is to support countries in implementing health-related Sustainable Development Goals. To achieve this, cooperation between the 13 participating organizations is to be improved. The WHO publishes an annual progress report on GAP activities.
Civil society actors have welcomed the GAP but also warn of the growing influence of private-sector actors in global health policy:
“We are concerned that the world could move further toward a privatized, undemocratic, and unjust global health policy.” (see: Agenda 2030: Where does the world stand?)
German Federal Government Strategy for Global Health
In October 2020, the German government adopted a new strategy to promote global health. The publication followed a long consultation process in which various stakeholder groups from science, business, civil society, and youth were asked for input. In this strategy, the “One Health” approach plays a central role and was intensely discussed. The incorporation of the “One Health” concept into international health policy is welcomed by NGOs such as VENRO.
For the decade up to 2030, five priorities are named:
- Promote health and prevention
- Work to mitigate the health impacts of climate change
- Strengthen health systems and ensure universal health coverage with non-discriminatory access for all
- Commit comprehensively and long-term to health protection, including protection against epidemics and pandemics, and continue engagement in humanitarian health aid
- Promote research and innovation in global health
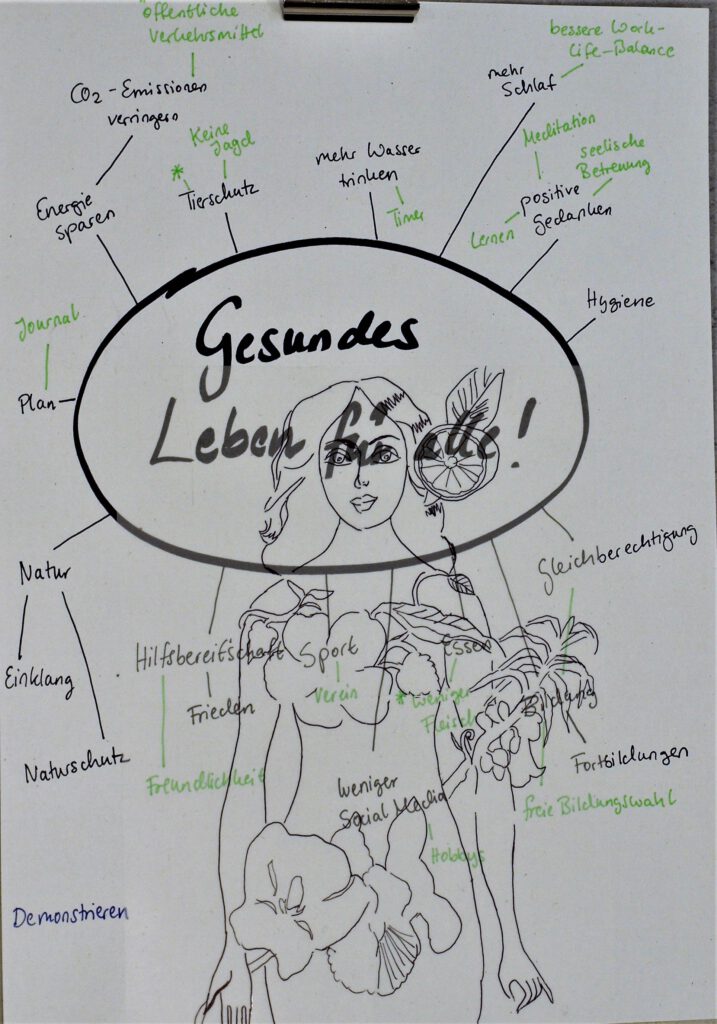
In June 2023, the German Advisory Council on Global Change (WGBU) published its main report “Healthy Living on a Healthy Planet.” The report examines the links between human health and environmental factors. The authors emphasize a broad understanding of health: holistic well-being requires resilient ecosystems and a stable climate. International development pathways must be found and implemented that treat humans and nature fairly. It is about healthy lifestyles that simultaneously protect nature—covering nutrition, exercise, and housing. It is about creating the conditions that enable such lifestyles. It is about preserving natural life-support systems—halting climate change, biodiversity loss, and global pollution—and preparing health systems for upcoming challenges while utilizing their transformative potential. Education and science are key to making the vision “Healthy Living on a Healthy Planet” a reality. Finally, international consensus on this guiding principle is crucial: without global cooperation, the vision cannot be achieved.
Get Involved: Initiatives Nationwide and in Hamburg
- Médecins Sans Frontières (Doctors Without Borders): provides medical assistance where urgently needed: in conflict zones, after natural disasters, and during epidemic outbreaks.
- Medico International: an international human rights organization supporting health projects in crisis areas and organizing solidarity campaigns.
- Health for Future: Health needs climate protection! H4F organizes healthcare professionals, students, and other stakeholders to advocate for climate- and health-oriented measures.
- Andocken: medical and social help for people without documentation.
- MiMi – With Migrants for Migrants (Hamburg): a project for intercultural health promotion, offering support in medical matters; intercultural health mediators provide multilingual guidance and explain essential aspects of the German healthcare system.
- Hamburger Arbeitsgemeinschaft für Gesundheitsförderung (HAG) e.V.: promotes socially-targeted health promotion and prevention in neighborhoods, families, kindergartens, schools, workplaces, and for older adults.
- Planetary Health Diet: a strategy for agriculture and nutrition to protect both human and planetary health.